Diagnosis of plantar heel pain
Pain on the bottom of the heel, referred to as plantar heel pain, is common and effects approximately 10% of the community. Plantar heel pain is a general term and can be used describe a range of different conditions that can effect the bottom of the heel. A suitably qualified health professional can help provide a specific diagnosis for pain in this region.
In most cases of plantar heel pain a person will experience:
- Pain on the bottom of the heel, most noticeable when getting out of bed in the morning, or after sitting for a while (this pain usually reduces after walking for a few minutes) (Figure 1)
- Pain at the end of the day, especially if you have been on your feet for long periods
On examination by a qualified health professional, there is regularly:
- Pain on palpation of the heel bone or calcaneus at a specific point called the medial tubercle (Figure 2)

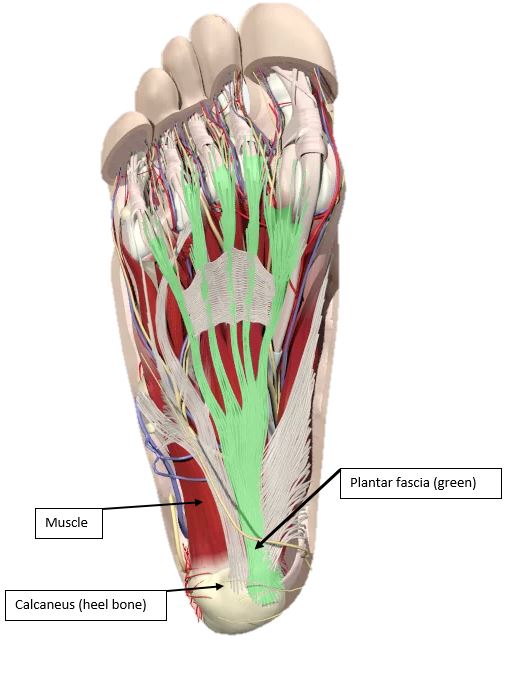
Diagnosis of your heel pain will most likely be called ‘plantar fasciitis‘, which has been used to describe inflammation of the plantar fascia where it attaches to the heel (Figure 3). However, in people that experience the symptoms listed above there a range of different tissues that might be effected including muscles, bone, fat and nerve structures – not just the plantar fascia. As such, we recommend that the term plantar heel pain be used unless a health professional has diagnosed something different.
Other terms that have been used to describe plantar heel pain include policeman’s heel, heel spur syndrome, jogger’s heel, plantar fasciopathy, and plantar fasciosis.
Other conditions that may cause heel pain
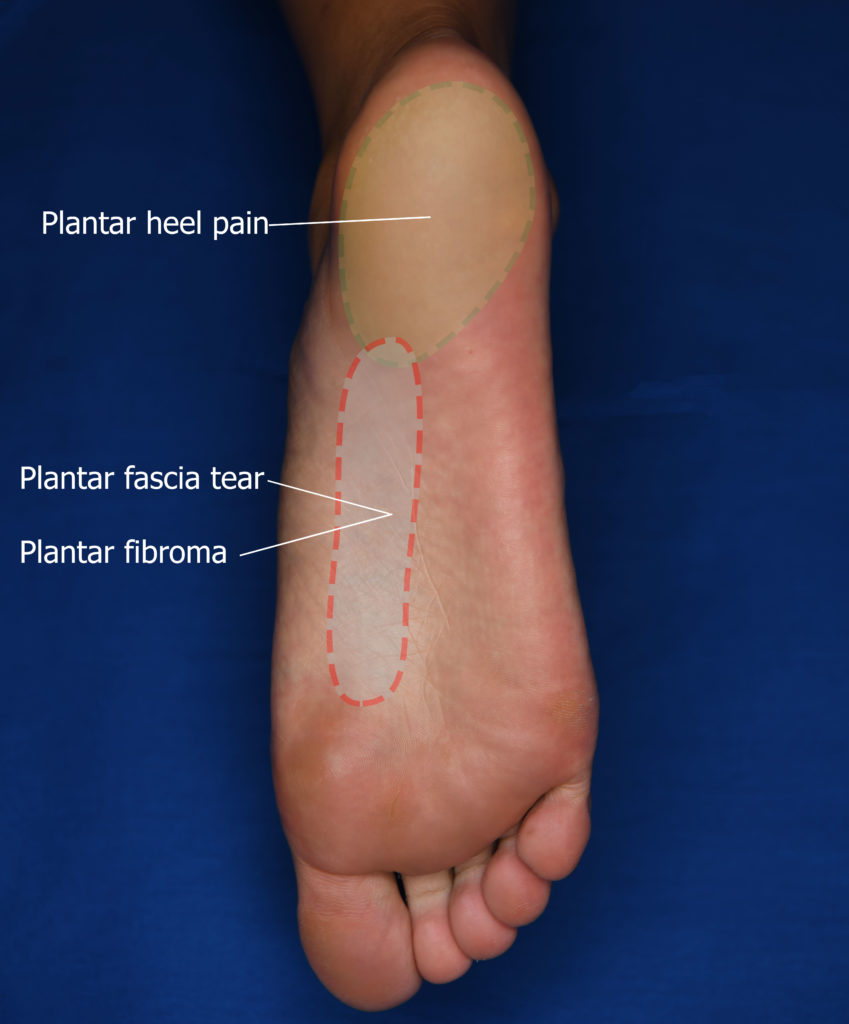
There are many other conditions that may cause pain on the bottom of the heel (Figure 3), such as:
- damage to the fat under the heel (fat pad syndrome)
- a compressed nerve under the heel
- a fracture of the heel bone (calcaneal (stress) fracture)
- a thickening of the plantar fascia (plantar fibroma)
These conditions may have symptoms that are slightly different to those of plantar fasciitis, however the symptoms can be very similar. A health professional (podiatrist, physiotherapist, GP) can assess and diagnose your heel pain. It is important you get a diagnosis, because the treatment may be different for each condition. Figure 4 highlights where pain is experienced for people with plantar heel pain and other related conditions.

Do I need imaging?
Imaging of the heel is generally not required to diagnose plantar heel pain. A diagnosis can be made based on symptoms and also an examination by a suitably qualified health professional.
In people with plantar heel pain, imaging can reveal multiple issues with different tissues including the plantar fascia, muscles, bone and fat pad. While imaging may be of use in understanding plantar heel pain, we do not know if it leads to better patient outcomes with different treatments. Importantly, findings found in imaging will most likely not explain the severity of pain that you are feeling.
We would recommend that if first-line treatment fails, or the diagnosis is uncertain, there may be a need for further investigations such as medical imaging. The most common forms of imaging for plantar heel pain are ultrasound and magnetic resonance imaging (Figure 5).

Links to research
Gamba et al. Relationship of plantar fascia thickness and preoperative pain, function, and quality of life in recalcitrant plantar fasciitis. Foot Ankle Int. 2018;39(8):930-934 (https://www.ncbi.nlm.nih.gov/pubmed/29696992)
